Each year, more than 800,000 Americans will suffer a heart attack. More than 150,000 will die before they experience their first symptom. Could they have been saved?
A relatively new and effective way to screen people at risk for heart disease is called coronary calcium scanning. Calcium scanning has been around since the late 1990s, and started capturing people’s attention when President Bill Clinton had his.
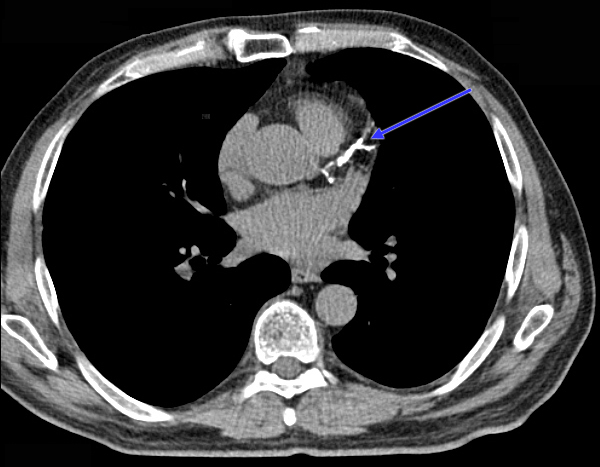
Coronary calcium screening uses specialized medical equipment to look at the structure of the heart’s coronary arteries. Much like standard x-rays, calcium scanning can be done using electron beam computed tomography (CT), multidetector CT (MDCT) or electron beam CT (EBT) scanners. The scanners are capable of taking more than 20 images per second. MDCT scanners are considered state of the art and can make it appear as if it has frozen the heart in time. After the test, radiologists examine the pictures taken and assign the results of the test an Agatston score that reflects the overall health of the coronary arteries. The scores range from 0 to 400; the higher the score, the more likely the patient has heart disease.
A Primer on Coronary Artery Disease
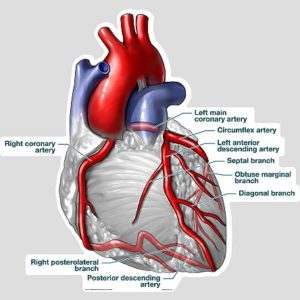
Coronary artery disease (often abbreviated CAD or CHD for coronary heart disease) begins early in life – almost from birth. Despite its function to supply blood to the body, the heart depends exclusively on coronary arteries to nourish it and keep it pumping – more than 115,000 times a day.
Early in life, the coronary artery’s lumen is free from disease with large internal diameters. As you age, the lumina begin to accumulate cholesterol and a soft, waxy substance called plaque. Some of these substances adhere to the inside of the lumen and flush themselves away in time. More serious is the plaque that begins to accumulate within the walls of the arteries, beneath the surface of the lumen, permanently narrowing the inside diameter of the arteries.
When the internal diameter of the lumen narrows enough to shut off circulation through the coronary arteries, people begin to experience angina, or chest pain. If the arteries are significantly clogged with plaque, the patient may suffer a myocardial infarction (MI), or heart attack. Often times, plaque can burst or break off, causing a blood clot that completely occludes arterial circulation. Depending on the severity of the MI, it can deprive the heart from oxygen-rich blood, causing permanent tissue damage.
Other times, arterial plaque can calcify, or become rigid, preventing the coronary arteries from expanding and contracting with normal blood pressure. Calcification can cause high blood pressure or lead to an MI.
Conditions that lead up to heart disease are called risk factors – behaviors or conditions that put you at risk for developing heart disease. They include:
- Hypertension
- High blood cholesterol
- Cigarette smoking
- Diabetes
- Obesity
- Sedentary lifestyle
- Family history
- Gender
- Age
Some risk factors like gender, age and family history for heart disease are impossible to control. Others, like hypertension (high blood pressure), high blood cholesterol, cigarette smoking, diabetes, obesity and living a sedentary lifestyle are modifiable, or under your control.
Coronary artery calcium scanning usually begins in the doctor’s office, before the patient begins experiencing symptoms of heart disease. Before recommending calcium scanning, your doctor may recommend simpler, easy to administer tests that include electrocardiograms (EKGs), stress testing, echocardiography, chest x-rays, and blood tests. In severe cases, patients may be rushed into the lab for coronary angiography or cardiac catheterization.
The topic of scanning usually comes up as an option in middle-age people who are wrestling with CAD risk factors – particularly those who have been told they should begin taking statin drugs to reduce their blood cholesterol level. Like most other drugs, statins often present unwanted side-effects, causing people to look for other solutions. Calcium scanning can help answer the question, “Do I have the beginning phases of coronary artery disease?”
The typical patient looking into coronary artery calcium (CAC) scanning is between the ages of 45 and 65. According to the American College of Cardiology and the American Heart Association guidelines, heart scans are generally not conducted on men younger than 40 or women below 50, because they are statistically less likely to have heart disease. They usually do not have calcium deposits in their coronary arteries. “But for a person without heart disease whose risk falls somewhere in the middle and who is trying to decide whether to take a statin, the results from a coronary artery calcium scan can be helpful,” says Dr. Ron Blankstein, an imaging specialist and cardiologist at the Harvard-affiliated Brigham and Women’s Hospital.